These education modules are for any staff member working within an interprofessional collaborative team caring for patients, resident or clients.
The goal of these learning modules is to complement and supplement present knowledge and support attitudes, skills, and behaviours to be effective team members and leaders within an interprofessional (IP) collaborative patient centred care team.
Module 1 and 2 (Introduction Module and Role Clarity module are to be taken together). After taking the two online modules, you will attend a classroom education session that will further expand on the concepts learned in the online modules.
There are three further online modules followed by 3 separate classroom sessions also.
Staff is requested to only take the module pertinent to an upcoming education session in a classroom setting in order to maximize knowledge.
This education offering consists of 5 modules:
Introduction
no one profession, working in isolation, has the expertise to respond adequately and effectively to the complexity of many service users’ needs
(CAIPE, 2008)
Interprofessional practice / collaboration (IPP/IPC) are not a new concept to some. For others it may be. This module discusses person centred care and the importance of communicating effectively in interprofessional teams. It is the first of 5 modules developed to enhance staff knowledge about interprofessional practice / collaboration.
Acknowledgement
Appreciation and thanks is extended to the following for permission to use content from their documentation to produce this Introductory Module on interprofessional collaboration/practice.
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework (2010).
- Canadian Interprofessional Health Collaborative: Resources toolkit. Copyright ©2009 All rights reserved.
- College of Health Disciplines and the Interprofessional Network of BC. The BC Competency Framework for Interprofessional Collaboration. © The University of British Columbia, all rights reserved.
- Healthcare Provider’s Practice Toolkit (September, 2010). The Enhance Ontario Project. Toronto, ON. HealthForceOntario.
- Mid Atlantic Renal Coalition. Communication Training Modules.
Thank you is extended to Kelly Lackie (BScN MN PhD(c) RN; Faculty/Interprofessional Education Lead, RN Professional Development Centre, Halifax, Nova Scotia) for reviewing the on line modules.
In this module “Client ” means Patient / Resident / Person
Learning Objectives
On completion of this module:
- Participant will be able to describe what interprofessional collaboration and interprofessional practice is.
- Participant will have increased understanding of what the competencies for Interprofessional Collaboration are according to the Canadian Interprofessional Health Collaborative (CIHC).
- Participants will have improved understanding of person centred care.
- Participants will have enhanced understanding of the importance of effective interprofessional communication.
What is Interprofessional Collaboration (IPC) and why is it important?
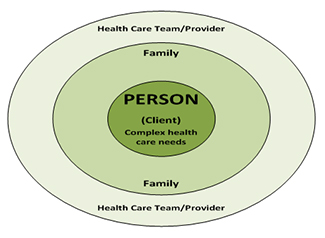
The Canadian Interprofessional Health Collaborative (CIHC) defines IPC as “the process of developing and maintaining effective interprofessional working relationships with learners, practitioners, patients/clients/ families and communities to enable optimal health outcomes” (CIHC, 2010, p. 6). The “PERSON” (patient/client /resident) is the focus – the reason for the formation of the team and is a full member of the team to the degree that they wish to be.
IPC is not a new term or way of thinking. In 1978, the World Health Organization (WHO) acknowledged that all health care workers needed to be trained to function as a team in order to respond to the health needs of the population as a whole (WHO, 1978).
Patient centered care was also at the center of attention as WHO suggests that individuals have the right and duty to be involved in the planning and implementation of their care (WHO, 1978).
In 2000, the Institute of Medicine released the comprehensive report, To Err is Human: Building a Safer Health System, which outlined the serious problem of healthcare associated error. In the US, these errors were equivalent to the number of deaths that would be caused by a 747 jet falling from the sky every day. In 2004, the Canadian Adverse Events study was released and indicated that 7.5% of all hospital admissions in Canada resulted in patient harm. This estimate did not extend to clients not admitted to hospitals and served in other care settings, so numbers may actually be higher. Further examination determined that large numbers of these errors could be prevented by improvements in communication and collaboration between providers (Kohn et al, 2000).
Evidence indicates that a lack of communication and collaboration between health providers can seriously harm patients(CIHC,2008,p.7)
What are some of the core concepts related to Interprofessional Collaboration (IPC)?
D’Amour et al., (2005) describe four core concepts that are commonly related to collaboration: sharing, partnership (teaming), interdependency, and power.7(p.8)
| Sharing |
|
| Teaming |
|
| Inter-dependency |
|
| Power |
|
The concept of Sharing includes the following: shared responsibilities, shared decision making, and a shared healthcare philosophy. Other effective strategies include shared values, data, planning and intervention, and professional perspectives.
Teaming (called partnership by D’Amour et al., 2005) implies two or more individuals (or organizations) who share a common set of goals and responsibilities for specific outcomes. A team is characterized by a collegial-like relationship that is authentic and constructive. Team relationships demand open and honest communication. Members treat each other with mutual trust and respect. Members must also be aware of, and value, the contributions and perspectives of the other team members.
Interdependency implies mutual and reciprocal reliance and dependence among all members of the care team that is characterized by a common desire to address each client’s needs. As a client’s need becomes more complex, expertise, contribution and participation is required from each member of the team. As a team works together and ‘gels’, the output of the whole becomes larger than the sum of the individual parts. The synergy then leads the team to collective action.
The fourth concept is Power. In an effective collaboration, power is shared among team members and characterized by “the simultaneous empowerment of each participant whose respective power is recognized by all...furthermore, such power is based on individual knowledge and experience rather than on functions or titles”. (D’Amour et al., 2005, p. 119 (as cited by 7)
What are the competencies for Interprofessional Collaboration (IPC)?
In 2010, the Canadian Interprofessional Health Collaborative (CIHC) released a framework outlining six specific competencies for IPC. Although these competencies are specific to individuals practicing in healthcare settings and the community, they can also be more broadly applied to organizations focusing on enhanced collaborative processes. The six competency domains are (CIHC, 2010):
- Interprofessional communication
- Person (Patient/Client/Family) - centred care
- Role clarification
- Team functioning
- Collaborative leadership
- Interprofessional conflict resolution 7 (p.9)
National Interprofessional Competency Framework
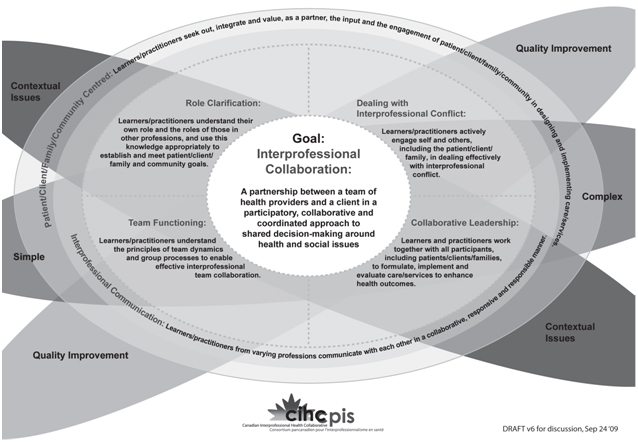
Interprofessional Collaboration

For interprofessional teams of learners and practitioners to work collaboratively, the integration of role clarification, team functioning, collaborative leadership, and a person-centred focus to care/services is supported through interprofessional communication.3
What is person-centred care?
According to the Canadian Interprofessional Health Collaborative (CIHC), 2009, person-centred care means that the patient/client (and their family, if applicable) is at the centre of their own health care.
Practicing person-centred care involves listening to clients and families and engaging them as a member of the healthcare team to the level of the client’s desire and comfort in making decisions. When the client is at the centre, the healthcare system revolves around their needs rather than the needs of healthcare providers, fiscal pressures or space allocation. However, person-centred care does not mean clients get exactly what they ask for, but rather that clients are working with their healthcare providers to determine health goals that are realistic, achievable and result in the best possible outcome for the client.
Person-centred care requires a balance between the professional knowledge of health care providers and the personal knowledge of the client and their family. Practicing person-centred care ensures the client is listened to, valued, and engaged in conversation and decision-making about their personal health care needs. It focuses on the client’s goals and the professional expertise of the team and adds the knowledge of all team members to the person’s self-knowledge and self-awareness.4
Providing person centred care in an interprofessional collaborative practice
According to Orchard (2010) interprofessional patient-centred collaborative practice is ”a partnership between a team of health professionals and a patient where the patient retains control over his/her care and is provided access to knowledge and skills of team members to arrive at a realistic team shared plan of care and access to the resources to achieve the plan” (p.249). An interprofessional collaborative practice offering person centred care does not mean that all the health care providers have to be present at all times. The most appropriate person will work with the client at the most appropriate time and ensure access and consultation between the patient and other collaborative team members when required.
Benefits of person centred care to staff and the client
| Benefits to Health Care Staff | Benefits to Client |
|---|---|
| Better health outcomes. (Research shows that the best results, as measured by adherence and outcome, come from a person who is informed and involved.) | Improved person-care outcomes. |
| Increased compliance of the client. | Increased self esteem of the client. Feeling better about themselves. |
| Fewer misunderstandings between the client/staff and staff. | Empowerment of the client to care for, and about, themselves. |
| Staff is more attentive. | |
| Staff is more understanding. | |
| Greater involvement of family and support system in the client’s care.7 |
| Medical Model | Person-Centered Model |
|---|---|
| Person’s role is passive (The client is quiet) | Person’s role is active (The client asks questions) |
| Person is recipient of treatment (The client doesn’t voice concerns, even if there’s a problem) | Person is a member of the team. |
| Provider (usually a doctor) dominates as decision-maker (The provider does not offer options) | Provider, who is based on the person's care needs, collaborates with the person (client) in making decisions. (The provider offers options and discusses pros and cons) |
| Disease-centered | Quality-of-life centered (The client focuses on family and other activities) |
| Provider does most of the talking (The provider may not allow time for questions) | Provider listens more and talks less (The provider allows time for discussion) |
| Person complies (or not) | Person (client) adheres to treatment plan (or not)8 |
Person: means client/patient/resident
Interpersonal & Communication Skills
To practice as a collaborative team practicing person centered care, effective communication is paramount.4
Effective interprofessional communication is dependent on the ability of teams to deal with conflicting viewpoints and reach reasonable compromises.2
Effective interprofessional communication requires the following of the team members:
- Consistently communicates sensitively in a responsive and responsible manner, demonstrating the interpersonal skills necessary for interprofessional collaboration.
- Effectively expresses one’s own knowledge and opinions to others involved in care.
- Demonstrates confidence and assertiveness to express one’s views respectfully and with clarity.
- Employs language understood by all involved in care and explains discipline specific terminology.
- Explains rationale for opinions.
- Evaluates effectiveness of communication and modifies accordingly.
- Actively listens and shows genuine interest in the perspectives and contributions of all team members.
- Is observant and respectful of non-verbal as well as verbal communication.
- Confirms that one understands all ideas and opinions expressed.
- Uses information systems and technology to exchange relevant information and keep team members updated in order to improve care.
- Is aware of and uses information resources from other professions.
- Plans and documents care on a shared health record.
Healthcare professionals are increasingly aware that interprofessional collaboration and effective team communication are essential for improved patient care and safety.1
A three-hospital study by Gawande et al. 2003 (as cited by 10) found that communication breakdowns between health professionals were responsible for 43% of surgical errors (p.351).
A growing body of descriptive and correlation evidence suggests that error rates are unnecessarily high (Baker et al., 2004; Tam et al., 2005), and highlight a relationship between poor communication between health professionals and poor patient outcomes (Alvarez & Coiera, 2006; Gawande et al., 2003; Risser et al., 1999)(as cited by 10,p.351).
The illustration below demonstrates why we need to communicate with each other. Lack of communication between health care providers does not instil confidence.5
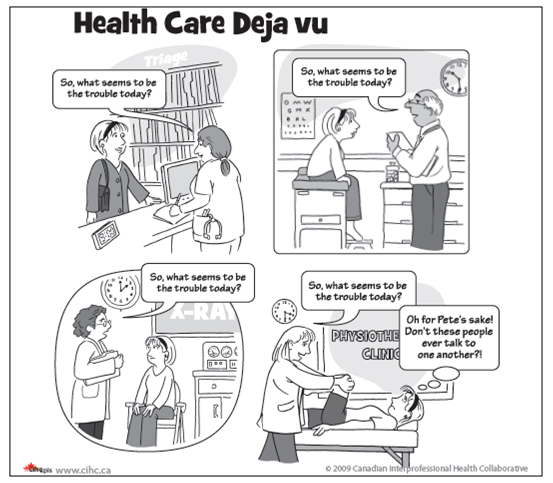
© 2008 Canadian Interprofessional Health Collaborative.
Person centred care and interprofessional communication are inter-woven into the remaining four competencies. Please review the education modules on the remaining competencies.
References
- Bajnok, I., Puddester, D., Macdonald, C. J., Archibald, D., & Kuhl, D. (2012). Building positive relationships in healthcare: Evaluation of the teams of interprofessional staff interprofessional education program. Contemporary Nurse: A Journal For The Australian Nursing Profession, 42(1), 76-89. doi:10.5172/conu.2012.42.1.76
- Canadian Interprofessional Health Collaborative. (2010). What is collaborative practice? IP Competencies - Interprofessional Practice Guide - Library and Academic Services at RRC Polytech
- Canadian Interprofessional Health Collaborative. (2010). A National Interprofessional Competency Framework. Retrieved from https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view
- Canadian Interprofessional Health Collaborative. (2009). What is patient-centred care? Retrieved from http://www.cihc-cpis.com/uploads/1/2/4/7/124777443/cihc_factsheets_pcc-2010.pdf
- Canadian Interprofessional Health Collaborative. (2008). Knowledge transfer and exchange in interprofessional education. Synthesizing the evidence to foster evidence based decision making.
- College of Health Disciplines, and the Interprofessional Network of BC. (2008). The British Columbia Competency Framework for Interprofessional Collaboration. Retrieved from http://www.chd.ubc.ca/teaching-learning/competency/bc-framework-interprofessional
- Healthcare Provider’s Practice Toolkit (September, 2010). The Enhance Ontario Project. Toronto, ON. HealthForceOntario. Retrieved from https://odha.on.ca/wp-content/uploads/2017/05/ENHANCE-Providers-Practice-Toolkit.pdf
- Mid Atlantic Renal Coalition (n.d.) Communication Training Modules: Module 2 Patient Centred Care p.4+p.14.
- Orchard, C. (2010). Persistent isolationist or collaborator? The nurse's role in interprofessional collaborative practice. Journal Of Nursing Management, 18(3), 248-257. doi:10.1111/j.1365-2834.2010.01072.x
- Rice, K., Zwarenstein, M., Conn, L., Kenaszchuk, C., Russell, A., & Reeves, S. (2010). An intervention to improve interprofessional collaboration and communications: a comparative qualitative study. Journal Of Interprofessional Care, 24(4), 350-361. doi:10.3109/13561820903550713
- World Health Organization. (1978). Declaration of Alma-Ata.
Proceed to the Role Clarity Module.
Introduction
This module and the education session in the classroom are provided to help individual health care providers clarify their role within the interprofessional collaborative team.
It is important for all health care providers to be aware of the different roles of each health care provider on a team, to learn about their individual perspectives and responsibilities for patient, client, resident care and to recognize and value the potential for role overlap.
Acknowledgments
Appreciation and thanks is extended to the following for permission to use content from their documentation to produce this module on Role Clarity.
- Baycrest: Baycrest Toolkit for interprofessional education and care.
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Facilitators Manual.
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework (2010).
- College of Health Disciplines and the Interprofessional Network of BC. The BC Competency Framework for Interprofessional Collaboration. © The University of British Columbia, all rights reserved.
- Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, D.C.: Interprofessional Education Collaborative.
- Winnipeg Regional Health Authority: Competency #2 Role Clarification.
Thank you is extended to Kelly Lackie (BScN MN PhD(c) RN; Faculty/Interprofessional Education Lead, RN Professional Development Centre, Halifax, Nova Scotia) for reviewing the on line modules.
In this module “Client ” means Patient / Resident/ Person
Learning Objectives
On completion of this module participants will have increased their knowledge of:
- Role Clarification.
- The Canadian Interprofessional Health Collaborative (CIHC) competency statement on role clarification.
- How role clarity works in the interprofessional collaborative team?
- The importance of understanding role clarity as a component of interprofessional collaboration.
- Potential members of the interprofessional collaborative team.
- The value that a variety of health care professionals contribute to the interprofessional team.
What is Role Clarification?
Health care providers must consider the roles of others; when working as part of a larger healthcare team. Along with understanding and describing their own roles, health care providers should be able to describe the roles and responsibilities of other health care providers.
When health care providers understand their role and are able to work to their full scope of practice it allows for the utilization of the most appropriate practitioner, provides a fair distribution of the workload and results in effective team functioning (CIHC, 2010). This understanding helps avoid duplication, improves team work and ensures more effective planning, implementation and evaluation of services.8
Role Clarification
Competency Statement: Health care providers, understand their own role and the roles of other health care providers, and use this knowledge appropriately to establish and achieve client / family and community goals.3
Competency Descriptors: Inter professional collaborative team members who understand and value the unique roles and responsibilities of various members of their health care team will demonstrate the following:
- Have sufficient confidence in and knowledge of one’s own discipline to work effectively with others in order to optimize client care;
- Demonstrates ability to share discipline specific knowledge with other health care providers;
- Negotiates actions with other health care providers based on one’s own role constraints and discipline specific ethical and legal practices;
- The ability to access other’s skills and knowledge appropriately through consultation;
- Recognizing and respecting the diversity of other health and social care roles, responsibilities, and competencies;
- The ability to perform their own roles in a culturally respectful way, and be able to shares one’s professional culture and values to help others understand one’s own point of view.
- Respects other team members’ professional culture and values in order to understand their point of view.
- Actively seeks out knowledge regarding others’ scopes of practice;
- Understands how others’ skills and knowledge compliment and may overlap with one’s own;
- Negotiates actions with other health care providers based on an understanding of other disciplinary role constraints, overlap of roles and discipline specific ethical and legal practices and;
- Integrating competencies/roles seamlessly into models of service delivery.3,5
Explanations / Rationale
Role clarification occurs when health care providers understand their own role and the roles of others and use this knowledge appropriately to establish and achieve client and family goals. Health care providers need to clearly articulate their roles, knowledge, and skills within the context of their clinical work. Each must have the ability to listen to other providers to identify where unique knowledge and skills are held, and where shared knowledge and skills occur. To be able to work to their full scope of practice, individuals must frequently determine who has the knowledge and skills needed to address the needs of clients to allow for a more appropriate use of health care providers and a more equitable distribution of workload.3
How does role clarity work in the interprofessional collaborative team?
Members of the interprofessional collaborative health care team recognize and respect the roles, responsibilities and/or competencies of all other team members. They:
- Respect the cultures of their community;
- Use appropriate language to communicate their roles, knowledge, skills, attitudes and judgement;
- Consult with others in appropriate ways to access their skills and knowledge; and
- Build professional and interprofessional competencies and roles in service delivery.
Demonstration of Role Clarification in Action
Following a serious road accident, several injured people are rushed to the emergency department (ED). The ambulance team has provided paramedical services, and now the ED team takes their reports and continues care. Injuries are severe, fatalities have occurred and the ED team is working at full capacity to manage this crisis. Physicians, nurses, respiratory therapists, social workers, spiritual care providers, housekeeping staff, porters and department clerks all need to be involved. Each team member must communicate effectively throughout the crisis while understanding how their roles complement or overlap one another. For example the social worker may need to collaborate with the spiritual care provider throughout the emergency stay so that the best possible treatment and support is provided.8
Learning about Roles & Responsibilities is key to collaboration
Learning about other professions is an important first step in collaboration. Many health care providers are unaware of the other health professions role due to a lack of collaboration during their respective education. In the course of their training, health care providers have a tendency to become socialized into their own professions and subsequently develop negative biases and naïve perceptions of the roles of other members of the health care team.
To practice effectively in an interprofessional health care team, however, one must have a clear understanding of other providers unique contributions: their educational backgrounds, areas of high achievement, roles, responsibilities and limitations.
Teamwork in a health care setting involves considerable overlap in competencies. Each health care provider should be knowledgeable of (and therefore comfortable with) the skills of the other health care providers. Moreover, an often overlooked member of the health care team is the client as well as their family. Health care providers must understand that the client and their family are integral members of the health care team with roles and responsibilities of their own.
From a clear understanding of others comes the basis for respect which underlies all successful collaborative endeavours. The need to establish the trust and respect of other team members derives from a central feature of collaboration:
No individual is responsible for all aspects of the client’s care, and therefore each member must have confidence that other team members are capable of fulfilling their responsibilities.2
Each health care provider's roles and responsibilities vary within legal boundaries; actual roles and responsibilities change depending on the specific care to be delivered. Non regulated team members roles and responsibilities vary depending on their work site. Health care providers may find it challenging to communicate their own role and responsibilities to others. For example, Lamb et al (2008) discovered that staff nurses had no language to describe the key care coordination activities they performed in hospitals. Being able to explain what other health care providers’ roles and responsibilities are and how they complement one’s own is more difficult when individual roles cannot be clearly articulated. Safe and effective care demands clearly defined roles and responsibilities.
Collaborative practice depends on maintaining expertise through continued learning and through refining and improving the roles and responsibilities of those working together.6
Why is it important to clarify skills, roles and responsibilities?
Health care providers from different disciplines/job categories are educated in their own unique professional environment and culture with its own language, terminology, problem-solving methods, behaviours, values and beliefs.
Because of this, many health care providers may not be familiar with the education base, the roles, or the range of functions of providers of other disciplines/job categories. This unfamiliarity with others can lead to under-utilization of skills and capabilities and to disputes about areas of overlapping practice within a team. Sometimes there is disagreement because the expectations and language create confusion.
Interprofessional collaborative team members from different disciplines bring a unique set of skills. Each member of the team needs to understand the unique expertise contributed by each member and the areas where knowledge and skills overlap. This understanding will contribute to mutual respect. Recognizing this overlap in competencies will help an interprofessional collaborative team determine who does what. By knowing the skills of other health care providers, team members can also refer clients more appropriately.
Failure to establish clarity of roles and to take advantage of the complementary skills of all team members can lead to frustration, conflict and inefficiency in service delivery.
To establish effective collaboration, it’s important to ensure that each provider on the team understands the role, scope of practice/employment and experiences of other health care providers in the team, and has the ability to articulate their own unique contributions.
A team focus identifies the clients problems from a holistic perspective:
- Medical issues and treatments
- Psychological/emotional issues and treatments
- Social issues and treatments
- Economic issues and treatments
- Living conditions and treatments7 (as cited by 1)

The client is central to any team
The need to address complex health promotion and illness problems, in the context of complex care delivery systems and community factors, calls for recognizing the limits of professional expertise and the need for cooperation, coordination, and collaboration across the professions in order to promote health and treat illness. However, effective coordination and collaboration can occur only when each profession knows and uses the others’ expertise and capabilities in a patient-centered way.
What do the Health Professionals on your team do?
Here are some examples of members of a collaborative team and their roles.
*This is not an all inclusive list*
| Team Member | Role and Responsibility |
|---|---|
| Dietitian |
Dietitians are food and nutrition experts who translate scientific, medical and nutrition information into practical individualized therapeutic diets and meal plans for people. They work with a variety of health professionals to manage nutrition for health promotion, disease prevention, and treatment of acute and chronic diseases. College of Dietitians of Ontario1 |
| Licensed Practical Nurse | A licensed practical nurse provides support and nursing services to clients, family members, and the community. According to the Canadian Council of Practical Nurse Regulators, “LPNs assess, plan, implement and evaluate care for clients throughout the life cycle and through palliative stages”. College of Health Disciplines British Columbia5 Licensed Practical nurses are most efficiently utilized in caring for patients with predictable (identified, unchanged, predictable) challenges and /or known health outcomes.10 |
| Medical laboratory technologist | Medical laboratory technologists perform lab tests on blood, body fluids, cells and tissues. MLTs in various specialties collect and process specimens, analyze results, and interpret findings. The knowledge and expertise of the MLT contributes to innovation in the prevention, diagnosis and treatment of diseases and medical conditions. The College of Medical Laboratory Technologists of Ontario (CMLTO)1 |
| Medical radiation technologist | Radiological technologists aid in the diagnosis of disease and injury by producing permanent images which are read by a physician who specializes in radiology. These images are captured on X-Ray film and other imaging devices such as video monitors, video tape and electronic digital imaging devices. The College of Medical Radiation Technologists of Ontario (CMRTO)1 |
| Occupational therapist (OT) | Occupational therapists help clients learn or re-learn to manage the everyday activities that are important to them, including caring for themselves or others, caring for their home, participating in paid and unpaid work and leisure activities. Occupational therapists address not only the physical effects of disability, injury or disease but also the psychosocial, community and environmental factors that influence function. College of Occupational Therapists of Ontario11 |
| Pharmacist | Pharmacists are experts in medication management. They are responsible not only for obtaining and dispensing medications, but also for their safe and effective use in the prevention of disease and the promotion of health and wellness. Ontario College of Pharmacists1 |
| Physician | Physicians assess the physical or mental condition of an individual and the diagnosis, treatment and prevention of any disease, disorder or dysfunction. College of Physicians and Surgeons of Ontario1 |
| Personal Care Worker (PCW) | PCWs do what a client would do for him or herself if physically and/or cognitively able. The role of a PCW depends upon the individual needs of the client, but can include home management, personal care, family responsibilities (routine care giving to children), and work, social and recreational activities. No regulatory body: For more information, visit Personal Support Network of Ontario1 |
| Physiotherapist (PT) | Physiotherapists are experts in physical rehabilitation. Physiotherapists assess physical function and treat, rehabilitate and prevent physical dysfunction, injury or pain, to develop, maintain, rehabilitate or augment function or to relieve pain. They assess the patient, establish a diagnosis for physical dysfunction, and then plan and implement an appropriate treatment program. College of Physiotherapists of Ontario1 |
| Registered Nurse | A registered nurses competency is based on five categories: professional responsibility and accountability, knowledge-based practice, ethical practice, service to the public, and self-regulation. Registered nurses promote health and the assessment of, the provision of care for, and the treatment of health conditions by supportive, preventive, therapeutic, palliative and rehabilitative means in order to attain or maintain optimal function. College of Nurses of Ontario1 Registered Nurses (RNs) are most efficiently utilized in caring for patients with complex (new, changed or complex) challenges and/or unknown health outcomes.10 |
| Respiratory Therapist | According to the “CSRT” Respiratory Therapists possesses a specialized body of knowledge, and base the performance of their duties on respiratory therapy theory and practice. They are essential members of the healthcare team, and assume a variety of roles in different areas of practice, such as clinical, education, health promotion, management, research, administration, and consulting. Respiratory therapists practice independently, interdependently, and collaboratively, and may practice within legislated professional regulations.9 |
| Social worker | In an interdisciplinary team, social workers provide the psychosocial perspective to complement the biomedical perspective. Social workers assess, diagnose, treat and evaluate individual, interpersonal and societal problems through the use of social work knowledge, skills, interventions and strategies, to assist individuals, families, groups, organizations and communities to achieve optimum psychosocial and social functioning. Ontario College of Social Workers and Social Service Workers1 |
| Speech-language pathologist (SLP) | SLPs prevent, identify, assess, treat and (re)habilitate communication and/or swallowing disorders. They also provide education and counseling services for people experiencing communication and/or swallowing difficulties. College Of Audiologists and Speech Language Pathologists1 |
| Unregulated health care worker | Contribute to the collaborative team depending on their job description and work site. |
Conclusion
To work in an intercollaborative team, members must understand their role in the team, the role of other team members and where overlap in practice may occur. This understanding will aid communication within the interprofessional collaborative team and will help develop and deliver patient/client centered care. Establishing clarity of roles will allow access to the complementary skills of all team members. This will help prevent frustration, conflict and inefficiency by ensuring the most appropriate person is providing the most appropriate care to the client requiring it.
There is an additional education session in a class room setting to help clarify the importance of appreciating the role that individual team members contribute to overall patient care. Understanding your role and the role of other health care providers is part of the process to function in an interprofessional competent manner. Role clarification will be explored further with other health care providers.
Please complete the online evaluation of this module. On completion you will be e-mailed a continuing education certificate for your continuing education portfolio.
References
- Baycrest, (2012). Baycrest toolkit for interprofessional education and care (IPE/C). Retrieved from https://www.baycrest.org/Baycrest/Education-Training/Centre-for-Learning,-Research-innovation/Our-Programs/Baycrest-Toolkit-for-Interprofessional-Education-a.aspx
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Facilitators Manual.
- Canadian Interprofessional Health Collaborative. (2010). A National Interprofessional Competency Framework. Retrieved from https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view
- College of Health Disciplines., & University of British Columbia. (2008). The British Columbia Competency Framework for Interprofessional Collaboration. Retrieved from http://www.chd.ubc.ca/teaching-learning/competency/bc-framework-interprofessional
- College of Health Disciplines., & University of British Columbia. (n.d.) What types of nurses are there?
- Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, D.C.: Interprofessional Education Collaborative.
- John A. Hartford Foundation Inc. (2001). Geriatric Interdisciplinary Team Training Program.
- Winnipeg Health Region: (2013) . Competency #2: Role Clarification.
- The Canadian Society of Respiratory Therapists. (n.d.) Standards of practice for respiratory therapists. Retrieved from https://www.csrt.com/rt-profession/
- Nova Scotia Department of Health, Professional Practice at Capital Health, College of Registered Nurses (CRNNS), College of Licensed Practical Nurses (CLPNNS) and the Registered Nurses Professional Development Centre (RN- PDC), (2010) Optimized Practice Optimizing the role of the RN, LPN and Assistive Personnel in acute care: A program to support the model of care initiative in Nova Scotia. MODULE: Core Concepts – Participant.
Introduction
This module and the education session in the classroom are provided to introduce participants to the principles, processes, values and techniques underlying effective interprofessional or collaborative teamwork in a health care settings and organization.
The overall goal of the Team Building online module and the classroom education session is to enhance participants’ knowledge, skills and confidence in leading and participating as members of interprofessional teams in health care.
Acknowledgments
Appreciation and thanks is extended to the following for permission to use content from their documentation to produce this module on Team Functioning.
- Baycrest: Baycrest Toolkit for interprofessional education and care.
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Facilitators Manual.
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Participants Manual.
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework (2010).
- Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, D.C.: Interprofessional Education Collaborative.
- University of Manitoba. (Module 3 A; Facilitators Guide. Interprofessional Practice Education in Clinical Settings: Immersion Learning Activities. Appendix 1.
Thank you is extended to Kelly Lackie (BScN MN PhD(c) RN; Faculty/Interprofessional Education Lead, RN Professional Development Centre, Halifax, Nova Scotia) for reviewing the on line modules
In this module “Client ” means Patient / Resident / Person
Learning Objectives
On completion of this module participants will have increased their knowledge of:
- The team functioning competency statement from the Canadian Interprofessional Health Collaboration
- The definition of a team?
- Phases of interprofessional collaborative team development
- How to establish an interprofessional collaborative team
- How to evaluate the interprofessional collaborative team
- Circumstances that favour the formation of interprofessional collaborative teams
- Advantages and Limitations of forming interprofessional collaborative team care
- Territoriality
- Key areas that an interprofessional collaborative teams must address
- Tools to improve communication within the interprofessional collaborative team
- Principles of effective interprofessional collaborative team meetings
- Steps to assist the interprofessional collaborative team to assess a client’s needs
Competency Statement on Team Functioning
From the Canadian Interprofessional Health Collaboration:
Health care providers understand the principles of team work dynamics and group/team processes to enable effective interprofessional collaboration.
Competency
To support interprovider/interprofessional collaboration, health care providers are able to:
- understand the process of team development
- develop a set of principles for working together that respects the ethical values of members
- effectively facilitate discussions and interactions among team members
- participate and be respectful of all providers’ participation in collaborative decision-making
- regularly reflect on their functioning with team practitioners, the client and their family
- establish and maintain effective and healthy working relationships with health care providers, the client and their family, whether or not a formalized team exists
- respect team ethics, including confidentiality, resource allocation, and professionalism.
Explanation/Rationale
Safe and effective working relationships and respectful inclusion of the client/family are characteristic of interprofessional collaborative practice. Collaboration requires trust, mutual respect, availability, open communication and attentive listening – all characteristics of cooperative relationships. Health care providers must be able to share information needed to coordinate care with each other and each client and their family and to avoid gaps, redundancies, and errors that impact both effectiveness and efficiency of care delivery. Complex situations may require shared care planning, problem-solving and decision making for the best outcomes possible.
In some situations, collaborative practice is undertaken via a formal interprovider/interprofessional team, requiring an understanding of team developmental dynamics, or practice in a micro-system, requiring awareness of how organizational complexity influences collaborative practice. Health care providers need to regularly reflect on their effectiveness in working together and also in achieving or meeting the needs of the client and their family.
Awareness of and commitment to interprofessional ethics unites all health care providers in the common goal of delivering the best care possible to the client, their family, and is fundamental to the ability to work together collaboratively.5
What is a Team?
small number of people with complementary skills who are committed to a common purpose, performance goals and approach for which they hold themselves mutually accountable.
Katzenbach, & Smith, 1994. 10 as cited by 3
Team Functioning
Learning about other health care providers is an important first step in collaboration. Many health care providers are unaware of what others “do” due to a lack of collaboration during their respective education. In the course of their training, providers have a tendency to become socialized into their own professions and subsequently develop negative biases and inaccurate perceptions of the roles of other members of the health care team. To practice effectively in an interprovider/interprofessional health care team, however, one must have a clear understanding of other members’ unique contributions: their educational backgrounds, areas of high achievement, and limitations. Teamwork in the health care setting involves considerable overlap in competencies. Each health care provider should be knowledgeable of (and therefore comfortable with) the skills of the other members. Moreover, an often overlooked member of the health care team is the client him- or herself, as well as the client’s family. As a member of the team, the client and other team members can develop the plan of care together. The intercollaborative team must include the client and their family by focusing on person (client) centred care.3
Team delivery of person (client) centred care.
Plan of care goals are developed in consultation with the rest of the team and therefore will be congruent with their expressed values. This requires the health care team to see the person as a full-fledged member of the team and therefore devote time in their assessment actively encouraging the client and their family to express their opinions, social circumstances and belief system. Communication should be open, non-judgmental and respectful and the client/family should be treated like they are an integral part of the interprovider/interprofessional team to the level they are comfortable with and in a supportive environment.
At times the client and/or family depend on the clinical team to guide them on specific and achievable outcomes especially for those decisions requiring clinical expertise and knowledge of diagnosis and treatment options. There are times when the clinical team identifies a problem area which the client/ family has not considered/does not consider a priority. A negotiation then follows between the client, their family and the team as to whether to address this area. If there are issues of client safety e.g. driving ability, financial abuse, the team members may have professional, legal or ethical duties which require them to address this area even if the client/family are not in agreement.
Phases of Interprofessional Collaborative Team Development
In order to help build a team, we need to remember that, like humans, teams develop through a series of stages. Probably the best-known model of team development is that of Tuckman (1965). (12 as cited by 3)
1) Forming
This is the very first stage of team development. Here team members meet for the first time, they determine their purpose, and they orient themselves to each other and the task as well as begin to establish trust between team members.
Key tasks at this stage are:
- to establish the goals of the team
- to learn about the skills and training of other team members
- to develop relationships based on mutual respect and shared goals
2) Storming
A key issue for teams is to effectively manage conflict while avoiding group think (i.e., where everyone blindly follows along and no one asks any questions). It is critical that teams balance both of these elements. Too much conflict can delay performance but too little conflict (i.e., group think) can stagnate creativity. So, in this stage, teams must determine how they will manage conflict, encourage differing views, and challenge the status quo.
Key tasks at this stage are:
- to develop effective means of role negotiation and conflict resolution for the team to progress to the next stage
- to develop methods of identifying problems with the team
- to re-evaluate initial goals, tasks and roles
- developing processes to overcome group think
3) Norming
Here the team starts to determine roles and responsibilities, sets and agrees on goals, develops operating guidelines for team functioning in their meetings and daily tasks, and determines the level of individual commitment needed to achieve the goals of the team.
Key tasks at this stage are:
- to establish the tasks and roles of team members
- to establish the mechanisms of communication
- to determine leadership and decision-making process
4) Performing
Once teams have reached this level, they are well-oiled machines. The key task at this stage is to maintain effective mechanisms for (1) continued communication, (2) conflict resolution, (3) continued goal and role re-evaluation, (4) evaluation of outcomes of team functioning, and (5) making the appropriate adjustments to the team. (13 as cited by 3)
Adjourning is the 5th level of group dynamics & occurs when the group no longer works together 11
A few notes of interest here:
- While scholars agree that teams go through four stages of development, there is some disagreement regarding the order of norming and storming. Some people argue that teams play nice first (i.e., norming) and then the issues of conflict emerge (i.e., storming); others argue that team’s storm first and then determine norms (see Whetten & Cameron for a discussion11). Either way, all scholars agree that all four stages are necessary for teams to be effective.
- Teams will cycle through these stages. Every time a new team member is added, the team will start back at stage 1. Note that teams develop in terms of both task processes and people processes (i.e., relationships) as they move from stage to stage.3
How to establish an Interprovider/Interprofessional Collaborative Team - Step by step guide
Step 1: Determine the Mission/Common Purpose4
- In 2 –3 sentences describes what the team is all about.
- Answer the following questions:
- What is the team’s role?
- Who are the key stakeholders?
- What are the CORE services offered by the team?
- What are the key challenges the team faces?
- The team checks to ensure that it includes members with the skills needed to achieve the purpose. If not, the team must seek out additional team members with the needed skills
Step 2: Performance Goals and Strategies
Based on the mission, have the team set 3-5 SMART goals. These goals must be:
- Specific
- Measurable
- Attainable (Hint: A good goal is difficult enough to challenge the team, but not so difficult that it cannot be attained)
- Relevant to the mission & recorded on paper
- Time-based
- Teams may choose to establish process or strategy goals. In both cases, you can complement longer term goals with shorter-term benchmarks.
Step 3: How will we evaluate and measure our goal progress?
- How is team effectiveness or success measured? Client health & functional status, use of provider time, satisfaction of team members/administrators / the client, costs, missed appointments, use of community emergency department services
- Which elements of the team approach lead to more effective outcomes?
- For which person is the team approach most effective?
- Under what conditions does the team operate most effectively?
Step 4: Determine roles and operating guidelines
The interprofessional collaborative team must determine roles, responsibilities & operating guidelines such as:
- Who is considered part of our team? Who are the team members?
- What are our expectations of each other?
- What is the role of the team leader?
- How does my role affect you?
- How does your role affect me?
- How does my role affect the team?
- How do we affect the person/client?
- How do we conduct effective meetings and how frequently?
- How will we share key information?
- How do we manage virtual team-members?
- How do we deal with conflict and foster an environment where people can present differing views?
- How do we address team members that are not ‘doing the right stuff’ and are hurting the team’s performance?
Step 5: Clear roles & operating guidelines: Why do we need them?
Clear roles and operating guidelines can help minimize the following ineffective interprofessional collaborative team behaviours:
- Team member disagreements
- Key work elements are missed (e.g, “Not my job.”)
- Multiple people doing the same work
- Decisions made in a vacuum (eg. some team members being left out of the decision making process)
- Blame game
- False agreement/group think
- Triangulation (e.g., there is a conflict between two people and they both ‘vent’ the issue at a third person)
Step 6: Create the plan
The final step is to take all the information collected in steps 1-5 and create a team charter. Plan should include sections on:
- Mission/common purpose
- Goals and measurement
- Operating guidelines
- Records of team meetings and decisions
Evaluating the Interprovider/Interprofessional Collaborative Team Process
Participation3
- Did each team member adequately participate in the discussion, contribute to the problem? To the care plan? (Important to take into account that each team member may not contribute to the discussion, or the team in the same way)
- Did team members express themselves clearly?
- Did team members follow-up/ask for clarification on vague comments or positions by others?
- Did the team process business in a way that allowed each member to contribute his or her viewpoint/role?
- Was there leadership to create the necessary structure and organization for the team to complete its business?
- Did leadership change based on needs?
- Was there adequate leadership for creating challenging and analyzing ideas?
Interprovider/interprofessional collaborative teams are established in order to provide collaborative care with client participation to the level they are comfortable with.
Circumstances that favour the formation of interprofessional collaborative teams
- the problems are complex enough to require more than one set of skills or knowledge
- the amount of skills or knowledge is too great for one provider
- assembling a group of health care providers will enhance the solution to the problems
- team-members can communicate on an equal basis
- all providers are willing to sacrifice some provider autonomy in working together for a common goal. (7 as cited by 3)
Principles of effective interprovider/interprofessional collaborative health care teamwork include the following:
- focus of members should be on needs of the client rather than on individual contributions of members;
- the basis of any health care team working collaboratively is communication with the client, a central principle shared by all health care providers;
- collaboration requires both, depending on others and contributing one’s own ideas toward solving a common problem;
- team members must respect, understand roles, and recognize contributions of their members;
- teams work both within and between organizations; (Grant 1995)
- Individuals may have improbable expectations of other team members which can lead to role ambiguity, role conflict, and role overload. (7 as cited by 3)
Advantages of forming an interprovider/ interprofessional collaborative team care
For clients:
- improves care by increasing the coordination of services
- integrates health care for a wide range of health needs
- empowers the client as an active partner in care
- can be oriented to serving clients of diverse cultural backgrounds
- more efficient use of time
For providers:
- increases provider satisfaction due to clearer, more consistent goals of care
- facilitates shift in emphasis from acute, episodic care to long-term preventive care and chronic illness management
- the collaborative experience enables the provider to learn new skills and approaches to care
- provides an environment for innovation
- allows providers to focus on individual areas of expertise
For educators and students:
- offers multiple health care paradigms to study
- fosters appreciation and understanding of other disciplines
- models strategies for future practice
- promotes student participation
- challenges norms and values of each discipline
For health delivery system:
- potential for more efficient delivery of care
- maximized resources and facilities
- decreases burden on acute care facilities as a result of increased prevention and client education interventions. (7 as cited by 3), (Baggs & Schmitt, 1997; Baker & Norton, 2004; Barrett, Curran, Glynn, & Godwin, 2007; Hendel, Fish, & Berger, 2007; Zwarenstein, Reeves, & Perrier, 2005),(as cited by 1)
- 82% of clients felt the quality of their health care experience was significantly improved when delivered by an interprovider/interprofessional team.6
Limitations of interprovider/ interprofessional collaborative team care
- process of team formation is time consuming & requires matching of schedules of different team members
- collaboration requires communication between team members, which takes time away from the client’s appointment in busy practices
- a comprehensive approach to health care may lead to increased use of limited services and resources
- a successful team requires on-going conflict resolution and goal re-assessment; failure of these tasks may impair health care delivery
- the interprovider/interprofessional collaborative team must also address issues of territoriality (7 as cited by 3)
Territoriality
A barrier to interprofessional collaborative teamwork is the problem of “turf battles.” These struggles over protecting the scope and authority of a profession involve issues of autonomy, accountability, and identity.
The principle of autonomy reflects the desire for each profession to define itself, to set its own criteria for practice and professionalism, and to maintain sole influence over its area of expertise. Loss of autonomy may lead to undesired changes in modes of practice and to loss of potential earnings.
Accountability, another key component of professionalism, refers to the evaluation and assessment of standards of care. Health care providers both define how they want to practice and are accountable to others in their profession for practicing according to these standards. Collaboration introduces performance evaluation by team members from other professions, which for some individuals represents an invasion into their own professional domain.
Finally, identity as an individual practitioner is due in large part to the identity of the profession as a whole. Interprofessional collaboration, by blurring the margins that define the roles of the various professions, may also impact upon the identity of individual providers.3
The task of the collaborative enterprise is to identify and address these underlying factors that lead to territoriality and to thereby facilitate interprofessional collaboration.
Key areas that interprovider/ interprofessional teams must address
1) Integrated clinical care
- health care providers contribute co-ordinated decision-making and management skills
- division of labour is organized around common goals, and provider competencies with each provider contributing his or her expertise as needed
- outcomes and goals are regularly re-evaluated
- health care providers share responsibility for the client’s care, including shared responsibility for positive and negative outcomes
2) Open communication
- Client case discussions involve not only diagnosis and management, but also individual and family issues.
- the client and their family are actively involved in the discussion of care and are considered team members
- pathways of communication are ensured by the organizational structure
Healthcare providers can learn to communicate with each other, with the client, in ways that are effective and meaningful. This in turn, will lead to a reduction in harm, increased satisfaction for all providers and overall better outcomes for the client and their family.
If there were one aspect of health care delivery an organization could work on that would have the greatest impact on client safety, it would be improving the effectiveness of communication on all levels – written, oral, electronic .
(Croteau, JCAHO)
3) Providers trained in team concepts
- collaborative rather than delegative model is employed;
- team members have skills in communication, conflict resolution, and leadership;
- members understand the roles and expectations of others; and
- members are innovative and tolerant of change
4) Respect for other team members
- team members are open-minded and respectful of other disciplines; and
- providers recognize the contributions of other team members (7 as cited by 3)
Key areas the teams must address
Having decided to implement an interprovider/ interprofessional collaborative team model there is a need to navigate the team development phases, and achieve the definition of an effective team.
This requires that teams address several key issues. Moreover, an examination of these five questions can help one understand issues that may be helping, or hindering, the performance of a team. The following summarizes the key areas that teams must address. (7 as cited by 3)
1. What is the team’s direction?
Here the team must establish its common purpose and goals. These are critical as it gives the team a sense of purpose and provides direction. Remember that teams should periodically revisit their common purpose and goals, both to track success as well as to ensure that they are still relevant.
2. Who performs which tasks and with whom?
Here teams must determine the key tasks and who is responsible for which tasks. Remember, teams are made up of people with unique and complementary knowledge and attitudes/judgement and have mutual accountability for the end result. Thus, while health care providers' may have clearly assigned roles, there must be some flexibility here as health care providers will need to ‘pitch in’ and cross traditional role boundaries in order to perform effectively. As such, it may be more beneficial to develop effective ways of sharing some of the responsibilities and tasks rather than only assigning them to a single health care provider. In terms of roles, it is helpful to consider the following:
- role clarity vs. ambiguity (are expectations clearly defined?)
- role compatibility vs. conflict (do roles conflict?)
- role overload (can an individual meet all expectations?)
The decisions of who does what can be guided by provider availability, level of training, or team member preferences. As with the setting of goals, it is important to periodically review and revise team member roles as necessary.
3. Leadership and Decision-Making
An emerging pattern in many health care teams involves equal participation and responsibility on the part of team members with “shifting” leadership determined by the nature of the problem to be solved.
In developing a mechanism for making decisions, the team must address the following questions:
- What needs to be decided?
- Who should be involved in the process? Who has the knowledge, skill and/or attitude/judgement for dealing with the decision?
- What decision-making process should be used?
- Who will be responsible for carrying out the decision?
- Who needs to be informed about the decision?
It would be unnecessary to require every member of the team to be present and to contribute to every decision of the team. Clearly, decisions will be made by a subset of team members in a time-efficient manner. Effective decision-making within the context of a collaborative team requires a balance between involving the fewest number of members without compromising the validity of the decision.
4. What mechanisms are needed to facilitate high team performance?
Teams must establish clear guidelines concerning issues such as conflict resolution, sharing of critical information and ensure effective communication within the team.
Conflict Resolution.
Given the mixture of skills and backgrounds, and the complexity of interprovider/interprofessional collaboration, a diversity of views and differences of opinion are inevitable. It is important to recognize, however, that conflict is both necessary and desirable in order for the team to grow and thereby develop greater efficiency and effectiveness.
Sharing of information.
To provide effective, coordinated care, a team must have an efficient mechanism for exchange of information. At the simplest level, this requires the time, space, and regular opportunity for members to meet and discuss individual client cases.
An ideal system for communication would include:
- a well-designed record system
- a regularly scheduled forum for members to discuss management of client issues
- a regular forum for discussion and evaluation of team function and development, as well as related interpersonal issues
- a mechanism for communicating with the external systems within which the team operates
Tools to improve communication within the interprovider/ interprofessional collaborative team
Open lines of communication are necessary to effective teamwork. It is the way that teams achieve their objectives. Research by the Association of Ontario Health Centres, (2007) found that being able to communicate and discuss concerns both formally and informally was important to reducing the stress of the work. Casual face to face encounters provided support and assistance to team members in their roles. And, poor communication was identified as a barrier to resolving conflict.
- Reasonable people can—and do—differ with each other. No two people are the same. Diversity among team members enhances creativity.
- Learn as much as you can from others. Learning the various backgrounds, cultures, and provider values of others can enrich your own skills and abilities.
- Evaluate a new idea based on its merits. Avoid evaluating ideas based on who submitted them or how closely the mirror your own personal preferences.
- Avoid comments and remarks that draw negative attention to a person’s unique characteristics. Humor is a key factor in a healthy team environment but should never be used at the expense of another’s identity or self-esteem.
- Don’t ignore the differences among team members. The differences should be honoured and used to advance the goals of the team.2
Without effective communication, the client is left feeling that health care providers do not speak to each other.
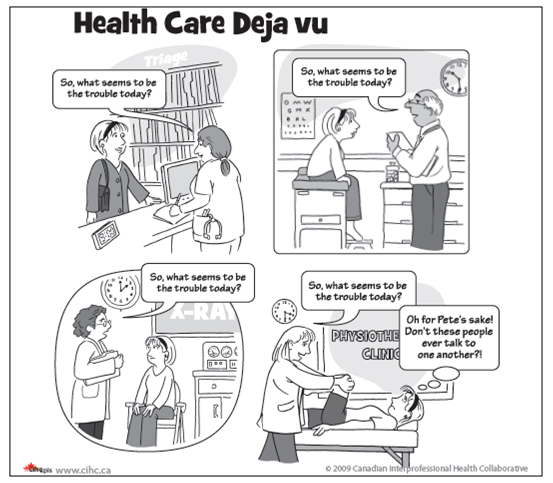
© 2008 Canadian Interprofessional Health Collaborative.
What is effective communication
Effective communication relies on team members listening and explaining their perceptions, and acknowledging and discussing their differences and similarities in views. Good communication means team members recommend and negotiate appropriate treatments for the person.
Barriers, such as differences in language and culture, can exist among team members and can make it difficult for one member to understand the meanings, intentions, and reactions of other team members. Our cultural heritage, sex, class, education level and stage of life influence our use of language and our perception of others. Team members must be aware of these differences in order to effectively communicate with each other as well as with the client and their family members.
Team members also need to recognize and value the different competencies and approaches of different health care providers. The key to team success is to value the differences on the team and use such diversity to achieve the team’s common purpose. (9 as cited by 2)
Effective healthcare teams are of great importance for meeting client needs, which is only possible through co- ordinated efforts and reliable communication processes (Department of Health, 2001; Husting, 1996). We consider that for this to happen, all members of the healthcare team must be clear of their own and others value, share an identity as a care team and work interdependently – thus implementing an interprovider/interprofessional approach to care 11
The following tips are helpful for valuing diversity and improving communication on your team: (9 as cited by 2)
| Closed questions |
|
| Open questions |
|
| Minimal leads and accurate verbal following |
|
| Repetition |
|
| Paraphrasing and reflecting |
|
| Clarifying responses |
|
| Confrontation and honest labelling |
|
| Integrating and summarizing |
|
Team Meetings
Principles of effective Interprofessional Collaborative Team Meetings
Team meetings can be structured, however a team meeting can be as simple as a unit huddle, two - three health care providers discussing a client’s care in the office, around the quality board when they meet.
Guidelines for interprofessional collaborative team members to aid consensus at meetings
- Contribute to the discussion rather than defend their position
- Seek out win-win solutions that satisfy the needs/concerns of all team members
- Use active listening skills and summarize what others are saying
- Seek to get the rationale for a person’s view
- Avoid voting or averaging to get an answer
- Don’t be afraid to disagree – address your differences in terms of the idea being presented not the person
To ensure consensus on the interprovider/ interprofessional collaborative team, contemplate the following questions
- Has each team member been honestly listened to?
- Have team members listened and understood the views of others?
- Do team members seem supportive of the alternative being discussed?
- Can each person summarize the alternative?
- Has it been a while since any new opinions/views were presented?3
Steps to assist the interprovider/ interprofessional collaborative team to assess the client's needs
The following questions will assist the interprovider/interprofessional collaborative team to assess what whether the clients' needs are being addressed. Considering the client’s medical, emotional, social, environmental and economic needs, answer each of the following questions:
- What is the overarching goal? At least three perspectives need to be considered and reconciled:
- client
- his/her family
- team
2) What are the client’s problems? (e.g. medical, emotional, social, environmental and economic).
3) What is the impact of each problem on the client’s health?
4) What strengths and resources does the client have or can be mobilized to deal with each problem?
5) What additional information is needed to adequately define the problem or its implications?
6)Who is involved in developing the plan of care? (What needs to be done; who will do it; when will it happen?)
7) What outcomes should be expected for each problem? (e.g. expressed in measurable terms, appropriate time to look for the outcomes) (8 as cited by 3)
Conclusion
This module was developed to assist with knowledge of “team functioning” in an interprovider/interprofessional collaborative environment. A definition of what a team is, its characteristics and key principles were supplied. Information of circumstances that favour interprovider/interprofessional collaborative team formation was given and advantages and limitations to team care were mentioned.Each team will be established according to their established need. Suggestions were provided to assist this process. An effective functioning interprovider/interprofessional collaborative team is essential to the delivery of effective care by the right person in the right place at the right time.
There is an additional education session in a class room setting to assist learning about team functioning from and with other health care providers.
Please complete the online evaluation of this module. On completion you will be e-mailed a continuing education certificate for your continuing education portfolio.
References
- Bajnok, I., Puddester, D., Macdonald, C. J., Archibald, D., & Kuhl, D. (2012). Building positive relationships in healthcare: Evaluation of the teams of interprovider staff interprovider education program. Contemporary Nurse: A Journal For The Australian Nursing Profession, 42(1), 76-89. doi:10.5172/conu.2012.42.1.76
- Baycrest, (2012). Baycrest toolkit for interprofessional education and care (IPE/C). Retrieved from https://www.baycrest.org/Baycrest/Education-Training/Centre-for-Learning,-Research-innovation/Our-Programs/Baycrest-Toolkit-for-Interprofessional-Education-a.aspx
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Facilitators Manual.
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Team Building: Participants Manual.
- Canadian Interprofessional Health Collaborative. (2010). A National Interprofessional Competency Framework. Retrieved from https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view
- Casimiro, L., Hall, P., Archibald, D., Kuziemsky, C., Brasset-Latulippe, A., & Varpio, L. (2011). Barriers and enablers to interprovider collaboration in health care: Research report. Beaulieu Consulting Inc
- Grant, R.W, Finnocchio,. L.J, and the California Primary Care Consortium Subcommittee on Interdisciplinary Collaboration. Interdisciplinary Collaborative Teams in Primary Care: A Model Curriculum and Resource Guide. San Francisco, CA: Pew Health Professions Commission, 1995.
- Hyer, K., Flaherty, E., Fairchild, S., Bottrell, M., Mezey, M., Fulmer, T., et al. (Eds.). (2003). Geriatric Interdisciplinary Team Training: The GITT Kit (2nd ed.). New York: John A. Hartford Foundation, Inc.
- John A. Hartford Foundation Inc. (2001). Geriatric Interdisciplinary Team training Program.
- Katzenbach, J. R., & Smith, D. K. (1994). The Wisdom of Teams. New York: HarperCollins. (p.45)
- Reeves, S., Goldman, J., Gilbert, J., Tepper, J., Silver, I., Suter, E., & Zwarenstein, M. (2011). A scoping review to improve conceptual clarity of interprovider interventions. Journal of Interprovider Care, 25, 167-174. doi:10.3109/13561820.2010.529960
- Tuckman, B.W. (1965). Developmental sequence in small groups. Psychological Bulletin, 63, 384-399.
- University of Manitoba. (Module 3 A; Facilitators Guide. Interprofessional Practice Education in Clinical Settings: Immersion Learning Activities. Appendix 1.
- University of Toronto. (2006). Educating health professionals for interprofessional care: becoming a leader in Interprofessional Education. Toronto: Author
Introduction
Conflict is a bi-product, a natural consequence, of people interacting with one another. It is natural; it is unavoidable and can have very positive consequences when handled properly.
Conflict is neither good nor bad, it is actually neutral. How we handle conflict will best determine whether it becomes a destructive or a constructive force in our relationships? If we handle it effectively, we may begin to see that conflict holds the potential for constructive outcomes.
This module and classroom session will provide you with information / tools to assist with conflict resolution.
Acknowledgments
Appreciation and thanks is extended to the following for permission to use content from their documentation to produce this education module on Interprofessional Conflict Resolution.
- Association of Ontario Health Centres. Building better team: A toolkit for strengthening team work in community health centres; Resources, tips and activities you can use to enhance collaboration.
- Baycrest: Baycrest Toolkit for interprofessional education and care.
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Conflict Resolution: Participants Manual.
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework (2010).
- Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Participants Guide. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author
- Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Power Point Slide Presentation. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author.
- University of Manitoba. (Module 3 A; Facilitators Guide. Interprofessional Practice Education in Clinical Settings: Immersion Learning Activities. Appendix 1.
- Winnipeg Regional Health Authority: Competency #6: Interprofessional Conflict Resolution.
Thank you is extended to Kelly Lackie (BScN MN PhD(c) RN; Faculty/Interprofessional Education
Lead, RN Professional Development Centre, Halifax, Nova Scotia) for reviewing the on line modules
In this module “Client ” means Patient / Resident/ Person
Learning Objectives
On completion of this module participants should have knowledge of the following:
- The definition of conflict.
- The conflict cycle.
- The competency statement from the Canadian Interprofessional Health Collaborative on interprofessional conflict resolution.
- What interprofessional conflict resolution is.
- Potential sources of conflict in the interprofessional collaborative team.
- Approaches to resolve interprofessional conflict.
- What are your personal triggers.
What is Conflict?
According to the New Oxford American Dictionary conflict is:
A serious disagreement or argument; an incompatibility between two or more opinions, principles, or interests.
Conflict is unavoidable in an interdisciplinary team environment. Conflict can occur between individuals or within the entire team, and it can arise because of a number of things. For instance, various health care providers on a team have differing professional perspectives that affect their relationships with each other, as well as with the person they are caring for. Team members also have different personalities that influence interactions among team members. A situation becomes a conflict because of people’s reactions to the circumstances or actions of others. These reactions are based on learned values, biases and lived experiences.
Within a health care team, there is considerable social pressure to avoid conflict—taking the time to work through team conflict may be viewed as taking time “away” from the person. But, avoiding conflict can be much more destructive to the team as a whole. Conflict should not be avoided, rather, it should be managed in a way that is constructive and can help move the team forward.(8 as cited by 1)
The Conflict Cycle6 (p.5)
The following represents the four stages of the Conflict Cycle:
| Stage 1 | Issues | An issue emerges that results in a difference of opinion, principles or interests |
| Stage 2 | Triggers | Something occurs that results in one or more parties becoming emotionally engaged |
| Stage 3 | Behaviours | Conflict is recognized and conflict resolution strategies are engaged |
| Stage 4 | Consequences | If appropriate strategies are used, the issue is resolved without damaging relationships |
| Issues | Two employees arrive for a meeting in the same meeting room – neither having reserved it. |
| Triggers | One employee suggests that since her meeting is more important the other person should reschedule. |
| Behaviours | After discussion they agree since both meetings are important, one meeting will be held in the larger of their offices. |
| Consequences | Both employees agree that this incident could have been avoided by reserving the meeting room. |
Adapted from Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Participants Material. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author(p.5)
Competency Statement
Competency Statement on Interprofessional Conflict Resolution from the Canadian Interprofessional Health Collaborative:
Health care providers actively engage self and others, including the client and their family by positively and constructively addressing disagreements as they arise.
Acknowledging that different perspectives – which may involve differing philosophies, beliefs and areas of expertise – can contribute to role ambiguity, role overload and goal differences is a start. Potential trigger areas – such as different treatment approaches, diagnosis, and input from people, goals and discharge plans – where tough conversations may be needed may vary from situation to situation. An individual being self-accountable and accepting responsibility for their ability to address conflict in a healthy, respectful way is an integral part of interprovider/interprofessional conflict resolution.4
Descriptors4
To support interprovider/interprofessional collaborative practice, team members consistently address conflict in a constructive manner by:
- Valuing the potential positive nature of conflict;
- Recognizing the potential for conflict to occur and taking constructive steps to address it;
- Identifying common situations that are likely to lead to disagreements or conflicts; including role ambiguity, power gradients, and different goals;
- Knowing and understanding strategies to deal with conflict;
- Setting guidelines for addressing disagreements;
- Effectively working to address and resolve disagreements, including analyzing the causes of conflict and working to reach an acceptable solution;
- Establishing a safe environment in which to express diverse opinions, and
- Developing a level of consensus among those with differing views; allowing all members to feel their viewpoints have been heard no matter what the outcome.
Explanation/Rationale4
To enable interprovider/interprofessional collaboration it is essential for health care providers, the client and their family to know how to deal with disagreements amongst themselves.
“Conflict positive” is a term that may be used to interpret difference of opinion as healthy and to be encouraged as constructive interactions. The events that lead to difference of opinion can come from positive and negative sources. Conflicts can arise from a number of sources:
- Roles: these arise over differing accountability issues, perceptions of role overloads or role ambiguity among health care providers.
- Goals: differences related to goals can arise because of dissimilar philosophies towards care, personal religious/spiritual beliefs, and professional socialization that includes differing approaches to care.
What is interprovider/interprofessional conflict resolution?
interprovider/interprofessional conflict resolution happens when healthcare providers work as a team that actively engages in addressing disagreements and responds effectively to all types of conflict.8 The word “conflict” has a negative connotation for many people; however, if properly managed, conflict may have constructive and positive outcomes.5(p.3)
Wouldn’t it be nice if all the members of a team treated each other respectfully at all times, agreed on everything, knew and accepted their roles from the outset, had no conflict and no stress? That’s a world most of us will never live in. In reality, after a team has its honeymoon period at the outset, the often untidy process of storming through the gritty details of leadership, purpose, traction speed, roles rules and regulations and all other housekeeping issues rears its head. This is part of the normal, unavoidable series of stages that all teams encounter
(Coles, 2007-2013). 5 (as cited by 9, p.16)
Potential Sources of Conflict in the interprovider/interprofessional collaborative team
- Individual values, beliefs, learned experiences, personalities, and philosophies of practice can create conflict. Each health care provider has their own values/beliefs/attitudes/customs/behaviours, diverse professional perspectives, and differences in modes/methods of practice. Lack of understanding of one’s role on the team may be perceived by the affected team member as lack of appreciation for his/her role on that team.
- Power imbalances that are often hidden and not acknowledged.
- Poor communication.
- Scarce resources (money, time, staffing, space).
- Organizational or professional change that poses a threat.
- Differing interests (concerns, hopes, expectations, priorities, fears).9
Conflict resolution is always challenging ... We all tend to shy away from conflict and sometimes conflict is good. Because it means that something is wrong and there needs to be change. So I think that a healthy team is sometimes going to experience conflict ... I think people just learning that conflict is a natural occurrence and not holding grudges.
(p. 60)3
Skills to assist team members respond to escalating conflict
Skills include:
Basic Assertion
This technique is possibly the simplest form of asking for what it is you want. Although challenging for those of us who tend toward passive communication styles, it is very effective when used in that it clearly and simply states our need/desire without qualification or excuses. To use this you simply use one of the following stems:
"I want …" or "I need …"
Examples: "I want to talk about what happened yesterday" "I need you to listen to me"
"I" messages
It is important to use the pronoun "I" to take responsibility and to promote cooperation and understanding when making statements to others. By starting off your statements with the pronoun "I", you are taking 100% responsibility for what you are saying, therefore promoting cooperation and understanding. You are also less likely to be threatening, especially to someone of higher authority.
Empathic assertion
Similar to active listening, empathic listening focuses on the feelings underlying the concerns a person is speaking to. Something as simple as "yes, that must be very frustrating for you" can have a powerful effect on a conversation and transform it into one where the person feels heard, understood and is willing to stop fighting as they see that you appreciate their feelings in the matter. Similar to reflection of feeling, this technique can be very powerful even when tensions are very high. It is crucial that we watch our tone and choice of words when using this approach, as a condescending tone will add fuel to the fire rather than transform the situation into a more positive experience. If we are genuine, we will communicate this and the other person will pick up on it.
Broken record
Sometimes it is effective to simply re-state your assertion. This can be done when another person appears to be reacting strongly to your statements or ignoring them for some reason. You simply repeat words in a calm voice. It is important to respond to legitimate points that are made by the other person and to pay close attention to your tone of voice.
Clarification
Clarifying responses help people understand the facts and the other person’s feelings and attitudes. Clarifying responses also help people think about what they have just said, examine their choices, and look at their life patterns.
Examples: "Is it possible that you feel …?" "Can you give me an example of what you are talking about?"
Probing and open questions
Open questions give people permission to say more about what they are thinking and feeling.
Examples: "What else can you tell me about …?" "Can you tell me more about…?" "What are some examples of the things you want to talk about today?"
Active listening
This technique is useful anytime and particularly when the other person is presenting in a very hostile manner. Active listening means you use verbal and non verbal cues to communicate to the other person that you are listening to their concerns. You focus on their concerns rather than your own. You can combine this with paraphrasing to really hear the other person - remember, when we feel heard, we often feel less of a need to force the issues. This is useful when someone is getting increasingly upset and it has the power to transform this experience into one of being heard and in turn, acts to de-escalate the situation.
Integrating and summarizing
Integrating and summarizing help ensure that the main concerns are understood. They help team members clarify their thoughts and feelings and encourage them to further explore confusing and conflicting issues.
Intent-action-effect
This is a useful technique for clarifying our messages to others. This approach is based on the belief that we may intend to communicate one message, yet unintentionally communicate a different message. Or more often than not, the observer interprets our message in a way that was not intended. This can occur either because of mixed messages on our part or a misinterpretation on the observer’s part. Either way, it can lead to more conflict. To use it, you simply clarify your intention; it can be very helpful to apologize for any mis-communication as well.
Confrontation and honest labelling
Confrontation and honest labelling are techniques for gently exploring uncomfortable subjects such as distortions of reality or differences between words and actions.
Examples: "I hear anger in your voice …" or "You sound sad even though you say everything is fine."
Restating content respectfully
This technique is especially effective for ensuring that you clearly understand what the other person is saying or asking for. You simply repeat back to them what you heard and ask if this is correct. It serves to ensure that you understand the other person as well as communicating to the other person that they are being heard. It also gives you time to assess the situation. When we are in conflict, feeling heard can often transform the situation into a less negative encounter on both sides. 2
Respectful interprofessional communication incorporates full disclosure and transparency in all interactions with others including the person and their family. All team members enact interprofessional communication that is consistently authentic and demonstrates trust with health care providers, the person and their family.3
Reflecting feeling
Communicates your understanding of how the person is feeling. Also provides the other party the opportunity to hear and reflect on their own experience.2( p.15-17)
Approach / Styles to resolve Interprovider/Interprofessional Conflict Resolution
Thomas and Kilmann identified two underlying dimensions to conflict-handling behaviour: cooperativeness (the attempt to satisfy the other person’s concerns), and assertiveness (the attempt to satisfy one’s own concerns). These two dimensions can be used to define five specific approaches or styles of dealing with conflict:(2, p.25+26)
Avoiding3 - uncooperative and unassertive (ie. Turtle):
Is hoping the problem will go away and not addressing the conflict. There is no attention to one’s own needs or those of the other. Avoiding might be letting an issue go, being diplomatic or simply withdrawing from a threatening situation. This tool is effective when time, place or personal health make it inadvisable to pursue discussion.
Characteristics
- Opposite of collaborating; one neglects his/her own concerns as well as those of the other person by not raising the conflict issue.
- Unassertive of self; uncooperative toward other.
- Issue is not addressed.
When to use
- An issue is trivial.
- There is no chance of getting what you want.
- The potential damage of confrontation outweighs the benefits of resolution.
- One needs to cool down, reduce tensions, and regain perspective and composure.
- The need is to gather more information.
- Others can resolve the conflict more effectively.
- The issue seems symptomatic of another fundamental issue.
Potential Consequences
- Decisions made by default.
- Unresolved issues.
- Energy sapped by sitting on issues.
- Self-doubt created through lack of esteem.
- Creative input and improvement prevented.
- Lack of credibility.
2(p.25+26)
Accommodating3 - cooperative and unassertive (ie. Teddy Bear):
Is meeting the concerns and needs of the other person and not addressing your own needs. This is giving in or yielding to the other person’s views. This style is used when you want to work co-operatively with the other person without trying to assert your own concerns.
Characteristics
- Opposite of competing; one who seeks to satisfy the other person’s concerns at the expense of one’s own.
- Unassertive of self; cooperative toward other.
- Issue is won by other, yielded by self.
When to use
- One realizes one is wrong.
- The issue is much more important to the other person.
- “Credits” need to be accumulated for issues that are more important.
- Continued competition would only damage the cause.
- Preserving harmony and avoiding disruption are especially important.
- Others need to develop and to be allowed to learn from mistakes.
Potential Consequences
- Decreased influence, respect, or recognition by too much deference.
- Laxity in discipline.
- Frustration as own needs are not met.
- Self-esteem undermined.
- Relinquished best solution.
2(p.25+26)
Competing3 - uncooperative and assertive (ie. Shark):
Is a strong style where the individual uses their power or control of the resources to assert his or her own needs. The style is helpful when an important principle or need is at stake. It can save time and get issues resolved.
Characteristics
- The opposite of accommodating; one uses whatever seems appropriate to win one’s own position.
- Assertive of self; uncooperative toward other.
- Issue is won by one party and lost by one.
When to use
- When quick, decisive action is needed.
- On important issues for which unpopular courses of action need implementing.
- On issues vital to organization welfare when one knows one is right.
- When protection is needed against people who take advantage of non-competitive behaviour.
Potential Consequences
- Eventually being surrounded by “yes” people.
- Reduced communication.
- Damage to relationship.
- No commitment from the other person.
- Having to keep “selling” or policing the solution during implementation.
2(p.25+26)
Compromising3 - intermediate in cooperativeness and assertiveness (ie. Fox):
Is looking for a mutually acceptable solution which somewhat satisfies both parties. You give up something, they give up something in order to come up with a solution you both can agree to. A compromise approach may work when you and the other person both want the same thing and you know you both can’t have it.
Characteristics
- Issue settled by splitting the difference; one seeks an expedient middle-ground position that provides partial.
- Satisfaction for both parties.
- Partially assertive.
- Partially cooperative.
When to use
- Goals are moderately important but not worth the effort of more assertive modes.
- Two opponents with equal power are strongly committed to mutually exclusive goals.
- Temporary settlements are needed on complex issues.
- Expedient solutions are necessary under time pressure.
- A back-up mode is needed when collaboration fails.
Potential Consequences
- No one fully satisfied.
- Short-lived solution.
- A cynical climate through perception of a sell out.
- Losing sight of the larger issues, ethics, objectives, values, and the organization welfare.
2(p.25+26)
Collaborating3 - cooperative and assertive (ie. Owl):
Is working toward solutions that satisfy the needs and concerns of both parties. This takes time to look at the all the issues and interests you both have which are behind the original positions. This approach combines the search for new alternatives and creating solutions that end in a “win-win” situation.
Characteristics
- The opposite of avoiding; one works with the other person to find a solution that fully satisfies both one’s own concerns and those of the other.
- Assertive of self.
- Cooperative toward other.
- Opposite of avoiding.
- Everyone’s interests are fully met.
When to use
- Both sets of concerns are too important to be compromised.
- The objective is to test one’s own assumptions or better understand the views of others.
- There is a need to merge insights from people with different perspectives on a problem.
- You need to increase commitment by including others’ concerns in a consensus decision.
- Working through hard feelings that have been interfering with an interpersonal relationship.
Potential Consequences
- Too much time spent on an insignificant issue.
- Can be time consuming.
2(p.25+26)
The context of the conflict will determine which style is more appropriate. Each style is useful and should be adapted for the presenting conflict
Constructive versus Destructive Conflict
Conflict that is appropriately and effectively managed can have positive or constructive outcomes.
Conflict that is poorly or ineffectively managed may have negative or destructive outcomes7 (slide 6)
Outcomes of Constructive Conflict7 ( slide 8)
- Improved understanding of issues
- Creative solutions to problems
- Relationships maintained and/or improved
- Resolution of tension & stress
- Enhanced problem solving skills
Outcomes of Destructive Conflict7 (slide 9)
- Unresolved problems or issues
- Damaged relationships
- An increase in tension & stress
- Reinforcement of differences
- Feelings of alienation & withdrawal
Adapted from Government of Nova Scotia Department of Health and Wellness (2009). Power Point Slide Presentation. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author. Slide 6,8+9.
What are your personal Triggers?
Triggers are typically statements, actions, gestures or behaviours that evoke an almost immediate emotional response. This emotional response reduces our ability to deal with an issue in a dispassionate way and frequently is the catalyst that causes conflict to escalate.
It is very important to recognize what your personal triggers may be, so that you can communicate to others that you are becoming engaged, and so that you can choose appropriate responses.
Often triggers are closely associated with our core values. The following is a list of common triggers. Review the list and identify the factors that could potentially trigger an emotional response from you.
It may be helpful to think about a situation where you became emotionally engaged very quickly.
How do you typically feel when something triggers or engages you in conflict?
If you are communicating with another person, what early warning signs may indicate to you that that something has triggered or engaged that person?
If triggers are not recognized and appropriately managed often conflict can very quickly escalate. Recognizing and addressing triggers often makes the difference between a conflict that has constructive outcomes and a conflict that has destructive outcomes.
Triggers can also arise from challenges to deep-rooted cultural values, beliefs and attitudes. We often don’t recognize this, because we perceive our own culture as “the norm.” The culture of “the other”, when it differs from our own, can be seen by some as inferior, less developed, morally wrong, etc and can elicit strong responses, generating conflict.6(p.6)
Adapted from Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Participants Material. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author (p.6)
Ambition
Assertiveness
Authenticity
Autonomy
Boldness
Collaboration
Compassion
Confidence
Consideration
Creativity
Decisiveness
Empathy
Fairness
Flexibility
Friendliness
Hard work
Honesty
Humility
Independence
Integrity
Learning
Loyalty
Openness
Optimism
Privacy
Productivity
Reliability
Respect
Sincerity
Straightforward
Thoughtfulness
Trust
An Interest Based Approach to Resolving Conflict
A typical process:
- Each person identifies their needs/interests
- The parties identify their shared interest
- Options for addressing this shared interest are considered
- An agreement is reached about the best option to meet this shared interest
Example 1:
Background Information
One-time special funding has enabled a collaborative practice to hire a summer student with a nursing background. There is a difference of opinion between the manager of the collaborative practice and one of the physicians as to the job responsibilities of the student. The manager of the practice identifies that she would like the student to spend the summer on a file clean-up project. This is a major project that even with a dedicated effort may not be able to be accomplished in the time available. The physician identifies that she would like the student to gather or develop take home materials for clients of the clinic. These materials could also be posted on the clinics website.
The Discussion
What are the goals of the clinic? (From a previous strategic planning exercise)
- To provide high quality health care services
- To increase the health and well-being of its clients
- To provide access to health care in a timely way
Given a new resource with a nursing background, what activities could contribute to meeting these goals?
- Developing or identifying materials for the website
- Developing or identifying materials for the person.
- Contacting patients who have not visited the physician in the previous 24 months
- Developing a process to minimize missed appointments
Outcome
- It was agreed that while file clean-up project was important there were other tasks (including some that had not previously been thought of) that were more closely aligned with the goals of the clinic. 6 (p.12)
Adapted from Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Participants Material. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author(p.12)
Example 2:10
Interprofessional conflict resolution in action
A team member in a leadership role consistently belittles other people in team meetings. People are very reluctant to attend the meetings and avoid interacting with that team member. The leader’s habits are so ingrained that a direct conversation with an administrator does not produce constructive results. The administrator talks to the other members of the team for concrete examples of what causes conflict in meetings and how to resolve it. This information is brought back to the leader. New ground rules of engagement are established, which help create a more functional and productive team while respecting the leader’s role.
A conflict positive perspective incorporates the idea that differences are a part of healthy, constructive interaction. In being self accountable when conflict arises, health care providers can aim to address and/or resolve the conflict, which creates a healthier environment for everyone.
Conclusion
This module was produced to provide the reader with information on interprovider/interprofessional conflict resolution. Conflict is inevitable within teams. How we deal with conflict when it arises is what is important. Potential sources of conflict within the team were identified as was the conflict cycle. Knowledge of what your personal triggers and conflict styles are may assist you to identify what factors trigger an emotional response in you. Skills were identified that may prevent conflict from escalating and approaches to conflict resolution were provided. Suggestions about when to use different approaches was given and also the advantages and disadvantages to each approach. Finally some examples of interprofessional conflict resolution in action were provided to demonstrate how a conflict situation can arise and how it can be dealt with.
There is an additional education session in a class room setting on interprofessional conflict resolution where this topic will be explored further with other health care providers.
Please complete the online evaluation of this module. On completion you will be e-mailed a continuing education certificate for your continuing education portfolio.
References
- Baycrest, (2012). Baycrest toolkit for interprofessional education and care (IPE/C). Retrieved from https://www.baycrest.org/Baycrest/Education-Training/Centre-for-Learning,-Research-innovation/Our-Programs/Baycrest-Toolkit-for-Interprofessional-Education-a.aspx
- Building a Better Tomorrow Initiative (BBTI). An Atlantic Provincial Primary Health Care Initiative. (Health P.E.I. Copy, 2009): Conflict Resolution: Facilitators Manual.
- Building Better Teams: A toolkit for strengthening team work in community health centres: Resources, tips and activities you can use to enhance collaboration. Reproduced with permission from The Association of Ontario Health Centres, Canada. Retrieved from www.aohc.org/index.php?ci_id=4139&la_id=1
- Canadian Interprofessional Health Collaborative. (2010). A National Interprofessional Competency Framework. Retrieved from https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view
- Coles, W.B. (2013). Strategies For Optimal Team Functioning - How To Reduce Conflict At Work. Retrieved from http://www.mentalgamecoach.com/articles/ReduceTeamConflict.html
- Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Participants guide. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author.
- Government of Nova Scotia Department of Health and Wellness (2009). Conflict Resolution: Power Point Slide Presentation. Building a Better Tomorrow Together: Team Development for Primary Health Care Collaboration. Halifax NS: Author.
- John A. Hartford Foundation Inc. (2001). Geriatric Interdisciplinary Team training Program.
- University of Manitoba. Module 3 A; Facilitators Guide. Interprofessional Practice Education in Clinical Settings: Immersion Learning Activities. Appendix 1.
- Winnipeg Health Region: (2013). Competency #6: Interprofessional Conflict Resolution.
Introduction
This module and the education session in the classroom are provided to help individual team members understand what it means to practice collaborative leadership and also identifies the characteristics of a collaborative leader.
Acknowledgements
Appreciation and thanks is extended to the following for permission to use content from their documentation to produce this education module on Collaborative Leadership.
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework (2010).
- Healthcare Provider’s Practice Toolkit (September, 2010). The Enhance Ontario Project. Toronto, ON. HealthForceOntario.
- KU Work Group for Community Health and Development. (1999). Chapter 13, Section 11: Collaborative Leadership. Lawrence, KS: University of Kansas. (Community Toolbox)
- Enhance Ontario (2010): Health Care Provider’s Toolkit.
- OHIO Department of Education: Community collaboration model for school improvement; Collaboration and collaborative leadership.
- Turning Point. Collaborative Leadership: Creating Clarity
- Winnipeg Regional Health Authority: Competency #4 Collaborative Leadership
Thank you is extended to Kelly Lackie (BScN MN PhD(c) RN; Faculty/Interprofessional Education Lead, RN Professional Development Centre, Halifax, Nova Scotia) for reviewing the on line modules
In this module “Client ” means Patient / Resident/ Person
Learning objectives
On completion of this module participant should have knowledge of the following:
- The competency statement on Collaborative Leadership from the Canadian Interprofessional Health Collaborative (CIHC).
- Fundamental concepts of collaboration and collaborative leadership.
- What collaborative leadership is.
- When collaborative leadership is appropriate.
- The reasons for practicing collaborative leadership.
- Outcomes associated with collaboration and other types of relationships.
- Potential issues with collaborative leadership.
- Who is a collaborative leader.
- How the collaborative leader practice.
- Elements unique to the practice of leading a collaborative process.
- Some final thoughts on collaborative leadership.
Competency Statement on Collaborative Leadership from the Canadian Interprofessional Health Collaborative
Learners/ practitioners understand and can apply leadership principles that support a collaborative practice model.
Descriptors
This domain supports shared decision-making as well as leadership but it also implies continued individual accountability for one’s own actions, responsibilities and roles as explicitly defined within one’s professional/disciplinary scope of practice. To support interprofessional collaborative practice, health care providers collaboratively determine who will provide group leadership in any given situation by supporting:
- work with others to enable effective client outcomes;
- advancement of interdependent working relationships among all health care providers;
- facilitation of effective team processes;
- facilitation of effective decision making;
- establishment of a climate for collaborative practice among all health care providers;
- co-creation of a climate for shared leadership; and collaborative practice.
Explanation/Rationale
Within collaborative or shared leadership, health care providers support the choice of leader depending on the client's needs and the competencies required to meet those needs at a given point in time. Health care providers assume shared accountability for the processes chosen to achieve outcomes. There are two components to the leadership role: task-orientation and relationship-orientation. In the former, the collaborative leader helps other members keep on task in achieving a commonly agreed upon goal, while in the latter, the leader assists members to work more effectively together (Heinneman & Zeiss) (as cited by 2,p.15).
In some cases, there may be two leaders-one for practitioners to keep the work flowing and the other who connects with the client/family in a helping relationship, serving as the link between the team and the client/family.2
Fundamental Concepts of Collaboration and Collaborative Leadership
Collaboration develops when health care professionals recognize that none can succeed without the others. Collaboration is the most complex type of relationship. It requires the most resources and takes the most time to develop. In collaboration, people network, communicate and cooperate. They share information, harmonize operations and activities, share resources and enhance each partner’s capacity (Gardner, 1999; Lawson, 2003; 2004: Lawson & Barkdull, 1999; Mattessich, Murray-Close, & Monsey, 2001). They also share power and authority; that is, they view themselves as equals (“all in the same boat”).
Most importantly, participating entities realize they are interdependent. They learn they cannot achieve their missions and goals without the contributions of the others (Lawson, 2003; 2004). For this reason, collaboration is characterized by lasting relationships characterized by high levels of a reciprocal investment, focus, trust, mutual commitment and a strong sense of joint ownership of positive outcomes for the person and their family. The facilitation of collaboration requires new types of leadership styles and structures. Collaborative leadership styles distribute power, authority and responsibility across the group. Leadership fosters shared commitments, helps resolve conflicts, facilitates lasting relationships and stimulates effective action. Collaborations also require new leadership, management and governance structures. Collaborative leadership structures involve team approaches rather than single person approaches. Team members collaborate, and their organizations develop firm partnerships in support of this new way of doing business (Rubin, 2002)8 (p.3.4).
What is Collaborative Leadership?
Collaborative leadership is about bringing together the appropriate health care providers with different views and perspectives, assisting them to set aside any self-interests, and providing an environment of trust where issues are openly and respectfully discussed in an attempt to find ways of helping each health care provider solve a larger problem or achieve broader goals. Collaborative leadership occurs when health care providers work together as a team with the client and his/her family to plan, introduce and evaluate care and services.
Collaborative leadership is really defined by a process, an inclusive culture that seeks to maximize the talents and abilities of the health care provider, where the leader ‘leads as a peer, not a superior13.
This style of leadership can be employed in almost any situation, but is seen more often in community-based health and human service organizations(6,para 7). It is a practical and an effective way to deal with clients with complex health care issues and challenges(13, p.335).
Collaborative leadership has the power to transform hospitals and healthcare organizations, improving the system today and for the future – to the benefit of clients, families and caregivers5.
Any member of the health care team can be the collaborative leader.
Traditional Leadership
Hierarchial/Top down
Few make decisions
Unilateral action
Win or shift power
Linear thinking
Programs & products
Charisma
Persuasive
Group falls apart if leader leaves
Collaborative Leadership
Self-governing
Broad participation
Guide & coordinate process
Build relationships
Systems thinking
Process
Vision
Empathetic
Group continues when leader leaves
7(slide 55)
Collaborative Leadership is not appropriate in health care when decisions have to be made quickly and health care providers have to act decisively to intervene in client care.
When is collaborative leadership appropriate?7
Collaborative leadership is appropriate when:
- Problems are serious and complex, and both affect and require attention from a number of health care providers and the client themselves. Clients with complex health care problems that no individual health care provider can resolve are situations when collaborative leadership is appropriate.
- There are a number of health care providers involved with varied interest. Collaborative leadership is needed to build trust among the health care providers/ the client and in the collaborative process itself. Practicing collaborative leadership ensures that each member of the health care teams opinion is heard and considered.
- An issue affects the whole health care organization. If large groups of health care providers are affected by an issue then collaborative leadership provides an opportunity for them to be heard.
Why practice Collaborative Leadership?7
Practicing Collaborative Leadership ensures:
Buy-in: Collaborative leadership encourages ownership of the enterprise, whether it's a health care organization, or a community project. By involving health care providers in decision making and problem solving, it makes what the health care provider is doing theirs, rather than something imposed on them by someone else. The sense of ownership builds commitment to the common purpose.
More involvement in implementation: Members of a collaborative health care team are more likely to be willing to take responsibility for implementing the team's action plan, because they were part of developing it.
Trust building: Collaborative leadership, by its use of an open process and its encouragement of discussion and dialogue, builds trust among the health care providers involved in the work in progress.
Elimination of turf issues: Collaborative leadership can help to address turf issues through establishing mutual trust, making sure each health care provider's concerns are heard, and helping organizations, factions, or individuals find common ground and work together to provide the best care for their client’s and their families.
Access to more and better information and ideas. When all health care providers are represented in an issue or party to addressing it, the health care providers bring with them a wealth of information, as well as a variety of perspectives. As a result, the solutions they arrive at are likely to be better than those developed in a vacuum, or by only a small number of people.
Better opportunity for substantive results: The combination of ownership of the process and its results, trust, real collaboration, and better planning yields real success in the real world. In looking at successful community development efforts, Chrislip and Larson,(as cited by 7) found that nearly all were characterized by collaborative leadership.
Generation of new leadership: Collaborative leadership in the health care setting helps to train new leaders from within the group, thus assuring continuity and commitment to the issues the collaborative health care team is addressing.
Organizational empowerment: The inclusion of appropriate health care providers - anyone with an interest or involvement in a health care issue - in problem-solving and decision-making not only prepares potential leaders, but leads to people taking more responsibility and caring more about what they do. It leads to better functioning in every sphere.
Fundamental change for the better in the ways a health care organization and its employees operate: Collaborative leadership breeds more collaborative leadership and more collaboration, leading to a different way of looking at solving problems. This in turn brings more willingness to find common ground and common cause with others, more willingness to tackle new issues, and more effective and wide-reaching solutions.
Outcomes Associated with Collaboration
Several researchers have documented significant benefits occurring as a result of collaboration and collaborative leadership.
Interprofessional collaboration (IPC) among healthcare providers has been identified as a key strategy to improve client outcomes.5 (p.1)
According to the Canadian Physiotherapy Association (2012), “inter-professional, collaborative, patient-centred practice benefits both clients and health care providers”.(p.2)
It has a positive impact on:3
- Population health and client care;
- Access and wait times;
- Communication, coordination of care and client safety;
- Recruitment and retention of health care professionals;
- Satisfaction among clients and health care professionals; and
- Health human resources.
A significant research base supports the benefits of inter-professional collaborative practice for clients with chronic conditions, such as diabetes and heart disease, for clients with mental health conditions, such as depression, and for geriatric patient populations (CAIPE,(as cited by 3).
Potential issues with Collaborative Leadership:5
- It's time-consuming. Collaboration takes time, and decision-making that involves a number of health care providers takes time.
- It demands the ability to face conflict directly. Collaborative leadership involves mediating a resolution acceptable to everyone. Collaborative leadership is not a job for people who like everything calm and who would prefer that no one ever raise their voice.
- It may mean trying to overcome resistance to the whole idea of collaborative leadership. Many health care providers would prefer a leader to tell them exactly what they need to do, so they know they're doing the right thing. Socialization in training makes some health care providers believe they should have ultimate control over patient care decisions and therefore do not feel the need to collaborate with other providers (Baker, Egan-Lee, Martimianakis & Reeves, 2011). Selling the concept of collaborative leadership may be the hardest part of the job.
- It can lead to groups taking what seems to you to be the wrong path. As a collaborative leader, you have to be able to let go of your own ideas and biases, and maintain a process that will guide the health care providers they collaborate with to their own goals, strategies, and action plans.
- It demands that leaders forgo their egos. You're not the boss in this situation, and furthermore, you may not get any credit if the group is successful.
What is a Collaborative Leader?
A collaborative leader is someone who safeguards and promotes the collaborative process.
There are two types of expertise that may be needed:
- Leadership that keeps people on task as they work toward the goal.
- Leadership that helps team members work well together.
In collaborative leadership, people receiving care can be leaders or the leadership can be shared amongst the health providers. As previously stated, one leader is responsible for the work flow and another leader provides a link between the client and the health care providers.7
The Collaborative Leader:
- Helps the team set norms that it can live by, and that encourage respect, participation, and trust.
- Assures that everyone on the team gets heard.
- Encourages and models inclusiveness.
- Helps people make real connections with one another.
- Mediates conflicts and disputes.
- Helps the health care team create and use mechanisms for soliciting ideas.
- Maintains collaborative problem-solving and decision-making.
- Pushes the health care team towards effectiveness by:
- Helps the inter professional collaborative team identify and obtain the necessary resources to do the work.
- Keeps the interprofessional collaborative team focused on what's best for the client/family, the organization and collaborative, as a whole, rather than on individual interests.7
Who are collaborative leaders?
Collaborative Leaders are people who:
- Have the necessary competencies to meet the clients health care needs.
- Have credibility within the health care organization, within their practice setting.
- Relate respectfully and easily to all members of the potential health care team.
- Have good facilitation skills.
- Can act as catalysts for the collaborative process.
- Nurture new leadership.
- Have a commitment to the collaborative, open process.
- Focus on the good of the organization, collaborative or health care organization as a whole.
- Forego the need to satisfy their ego.
- Encourage new ideas from others.
- Step aside, temporarily or permanently, when appropriate.7
Key Leadership Traits all Collaborative Leaders Share.
Bratton and Tumin (2012) as cited by (12, p.337) identified four key leadership traits that all collaborative leaders share. They are:
- Focus on authentic leadership; placing the goals of the health care organisation ahead of their own self-interest and following through on their commitments.
- Relentlessly pursue transparent decision making; making clear how their decisions are made and who is accountable for the outcomes within the health care team.
- View resources as instruments of action; realising shared goals through the flexible use of shared resources.
- Clarify the relationship between decision rights, accountability and rewards; taking time to establish decision paths and a common vocabulary for successful collaboration among the health care providers.
The best thing a collaborative leader can do is to lead by example. They have to ‘walk the talk’, and be seen to model the right behaviours(12, p.337).
You are a collaborative leader once you have accepted responsibility for building—or helping to ensure the success of—a heterogeneous team to accomplish a shared purpose.10
Elements unique to the practice of leading a collaborative process
Collaborative leaders should possess a number of critical skills and capacities. Six key elements unique to the practice of leading a collaborative process are as follows:
- Assessing the Environment for Collaboration: Understanding the context for change before you act.12 Assessing the Environment: This is the capacity to recognize common interests, especially the capacity to recognize and understand other perspectives. It is a fundamental quality of collaborative leadership. Collaboration seeks goal attainment around shared visions, purposes, and values. When he or she brings different points of views to an issue or problem, a collaborative leader facilitates connections and encourages group thinking that identifies clear, beneficial change for all participants. The goal is to set priorities and then identify barriers and obstacles to the achievement of priorities. This is the capacity to recognize common interests among health care team members and to understand their differences stances. Collaboration among the health care providers seeks goal attainment around shared visions, purposes, and values. The collaborative leader brings different points of views to an issue or problem. They facilitate building connections and encourages group thinking that identifies clear, beneficial change for all team participants. The goal is to set priorities and then identify barriers and obstacles to the achievement of those priorities.
- Creating Clarity – Visioning and Mobilizing: Defining shared values and engaging people in positive action.12 Having clarity of values is a quality that characterizes collaborative leaders. collaborative leaders seem to exhibit clarity of purpose, often about creating and sustaining a purpose. "Visioning and mobilizing", in relation to clarity of values, has to do with a commitment to a process or way of doing things.Often “mobilizing” refers specifically to helping health care providers/ team members develop the confidence to take action and sustain their energies through difficult times. Clarity leads to focus which leads to increased collaborative team energy (power). Often too little time is spent in the process of “informal exploring” to understand problems, thereby developing clarity, a shared vision can be inspiring. A shared vision for the health care team is a way to create clarity for the members.
- Building Trust:12 The capacity to promote and sustain trust is important in the collaborative process. If a collaborative leader fails to engender trust among participants, their involvement will wane, and the best ideas and innovative approaches will not be shared. The nature of the collaborative health care environment means that team members are equally valued and work closely together on a daily basis. This gives the opportunity for immediate feedback, praise and constructive criticism among members.( Jartese, para 19) Health care providers must feel able to offer their opinions in a safe and respectful manner.
- Sharing Power and Influence: Developing the synergy of the collaborative health care team to accomplish more.12 Sharing Power and Influence: The capacity to share power and influence is an uncommon trait among leaders. Society traditionally rewards individual achievement, but collaboration cannot be achieved through a solo effort. The new approach of collaborative leadership recognizes that power is greatest in a collaborative health care team. By encouraging equal participation across all levels, collaborative leaders allow solutions to develop from the best ideas among the health care providers and take a team approach to problem solving (Jartesh para 5). Rather than being concerned about losing power through collaboration, leaders need to see that sharing power actually generates power…that power is not a finite resource 7.
- Developing People: Committing to the development of people as your key asset through mentoring and coaching.12 Developing People: This practice is best described as a genuine concern for bringing out the best in others, maximizing the use of other people’s talents and resources, building power through sharing power, and giving up ownership or control. These are themes that relate to realizing and promoting the potential in other people. Coaching and mentoring creates power, which increases leadership capacities and builds confidence by encouraging experimentation, goal-setting, and performance feedback. Information, resources, knowledge, time and effort are shared. This allows roles and responsibilities to evolve and fluctuate based on the greater good.
- Self Reflection – Personal Continuous Quality Improvement: Understanding your own leadership, engaging others.12 Self-Reflection: The collaborative leader must use self-reflection to examine and understand their values and think about whether their behaviours are congruent with their values. At critical junctures in the collaborative process, through reflection, successful leaders make time to consider verbal and nonverbal communication within the health care team. They think critically about the impact their actions and words have on the health care team's progress toward achieving its goals. Great collaborative leaders have the ability to recognize the impact of their behaviour and adjust accordingly. All members of the collaborative team will benefit from using self reflection when working in a collaborative team environment
Final Thoughts
In the end, collaboration and partnerships entail a new way of doing business. The most important priority for you to keep in mind is that these new ways of doing business yield improved results for health care organizations, health care providers, and for the client and their family.
New ways of doing business also require new ways to lead, manage and govern, and collaborative leadership is the answer to these needs. As the boundaries of health care improvement expand, the collaborative health care team adds new members representing other professions and clients and their families. These new team members join with existing members to share responsibility and accountability for health care improvement processes and outcomes. These collaborative leadership teams, structures and processes are vital when multiple programs and services are being implemented simultaneously in several places and involving many organizations and people.
The distinctive advantage of this model is:
- The ability to affect multiple improvements simultaneously.
- It also highlights the limitations of “one person leadership and management”.
- In this new model, health care leaders leaders simply do not have to do it all, alone (and simply can’t). Collaborative leadership teams and structures enable coordinated and harmonized leadership, management and governance that cross the boundaries within the health care organization.
- These new working relationships respond to the needs of the client, and the various health care professionals collaborating on their care. All know firsthand the problems they encounter individually in trying to be all things to all clients.
- Collaboration, partnerships and collaborative leaderships thus offer new supports and resources for each team member, promising to maximize their effectiveness, prevent burnout and improve worker retention.
- Last, but far from least, the client and their families will be better served, especially when they are included in the collaborative team to the level they are comfortable with. The other benefits are no less important. Collaboration and partnerships promise to eliminate fragmentation, duplication and competition that often prevent participation. Furthermore, this new way of doing business promises to address heretofore unmet needs, including program and service gaps. As these needs are met, and as the gaps are bridged and filled, clients will benefit and in turn health care outcomes will see improved results8 (p.3.24).
Collaborative leadership is grounded in a belief that all of us together can be smarter, more creative, and more competent than any of us alone13 (p.336).
Conclusion
This module has provided you with information on what collaborative leadership is and when it is appropriate to use. Some fundamental concepts about collaboration and collaborative leadership were provided and outcomes associated with their use. Characteristics of collaborative leadership are listed and reasons to practice in this manner are discussed. Collaborative leadership is practiced to ensure the most appropriate provider is leading the team at the most appropriate time in order to deliver best person centered care.
There is an additional education session in a class room setting on collaborative leadership where this topic will be explored further with other health care providers.
Please complete the online evaluation of this module. On completion you will be e-mailed a continuing education certificate for your continuing education portfolio.
References
- Beinecke, R.H. (2013) Leadership for Wicked Problems ACMHA, 1-21. Retrieved from https://www.leaders4health.org/images/uploads/files/Beinecke_Wicked_Problems.pdf
- Canadian Interprofessional Health Collaborative. (2010). A National Interprofessional Competency Framework. Retrieved from https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view
- Canadian Physiotherapy Association. (2012). Position statement: Inter-professional collaboration and practice. 1-3. Retrieved from https://physiotherapy.ca/sites/default/files/positionstatements/inter-professional-collaboration_en.pdf
- Centre for Creative Leadership, (2007) What’s next? The 2007 Changing Nature of Leadership Survey. Survey retrieved from http://www.ccl.org/leadership/pdf/research/WhatsNext.pdf
- Enhance Ontario, (2010). Health care provider’s toolkit. 1-39. Retrieved from https://odha.on.ca/wp-content/uploads/2017/05/ENHANCE-Providers-Practice-Toolkit.pdf
- Heshka, L., Jeannot, G., McPhee, L., Radloff, J., Schommer, K., Weir, L. & Wollbaum, M. (2011). Leading Collaboration among the Providers of Primary Health Care; Saskatchewan Institute of Health Leadership. p.1-55. Retrieved from https://www.uregina.ca/cce/assets/docs/pdf/sihl/2010-11LeadingCollaborationamongtheProvidersofPrimaryHealthCare-march2011.pdf
- KU Work Group for Community Health and Development. (1999). Chapter 13, Section 11: Collaborative Leadership. Lawrence, KS: University of Kansas. Retrieved June 17, 2013, from the Community Tool Box: Retrieved from: http://ctb.ku.edu/en/table-of-contents/leadership/leadership-ideas/collaborative-leadership/mains
- Porter- O’ Grady, T. & Malloch, K. ( 2010). Innovation Leadership. Boston, Toronto, London, Singapore. Jones and Bartlett Publishers.
- Rubin , H. (2006) Through Others’ Eyes: A Collaborative Model of Leadership” The Heart, Mind, and Soul of Educational Leadership: Volume 2, Out of the box leadership, Paul Houston and Robert Cole (editors), Corwin Press.
- Turning Point (2006). Collaborative leadership; fundamental concepts. Power point presentation Slide 55.
- Turning Point. (2006). Collaborative Leadership Learning Modules: A Comprehensive Series.
- Wilson, S. S. (2013). Collaborative leadership:It's good to talk. British Journal Of Health Care Management, 19(7), 335-337.
- Winnipeg Health Region: (2013). Competency #4: Collaborative Leadership.
Your manager / resource nurse/ educator will advise you when to take the online module. It is intended that the online module be taken as close to the classroom education session as is possible for the practice area.
Continuing education certificates are provided to participants for their continuing education portfolios. The online module gives staff one continuing education hour and the classroom sessions provides staff with 2 – 2.5 hours of continuing education hours.
If you require further information, please contact dadewar@ihis.org